
The New Zealand Veterinary Association (NZVA) has as its goal that, by 2030, New Zealand will not need antibiotics for the maintenance of animal health and wellness. One may ask just how will this be achievable? Antibiotics have revolutionised the health and well-being of both humans and animals during the 20th century. But 96 years on from the discovery of penicillin in 1928, the effectiveness of antibiotics is declining. The decline in effectiveness and the emergence of ‘super bugs’ or antimicrobial resistance (AMR), is so great that the World Health Organization has suggested that antibiotic resistance is one of the greatest global health challenges facing mankind in the 21st century.
Why has this come about? The increasing rate of resistance to antibiotics and other disease-fighting agents (broadly coined “antimicrobials”), is largely due to the overuse of antibiotics in humans and livestock and the consequential ability of bacteria and other organisms to rapidly evolve to bypass the effects of these drugs. Clearly one solution would be to develop new classes of antimicrobials, but no new antibiotics have been developed in the last 30 years. Another would be to improve the stewardship of their use, which is the path being undertaken by the NZVA in the production of a document called “Antibiotic judicious use guidelines for the veterinary profession”. One of the significant developments in this document is a “traffic light” system which divides antimicrobials into 3 groups (green, yellow and red), with the red zone including the Critically Important Antibiotics. Their recommendation is that these red zone antimicrobials are used only after veterinary diagnosis and on a case-by-case basis.
The first vaccine was developed in 1796 by Edward Jenner. He realised that milkmaids who had previously caught cowpox did not appear to catch smallpox. He took material from cowpox blisters and inoculated it into another person’s skin. The culmination of vaccination was the eventual eradication of smallpox from the world. Using vaccines to prevent infections will reduce the need for antibiotics, which is where vaccines come into their own. Vaccines are the icon of prevention or the fence at the top of the cliff, whereas antibiotics could be thought of as the ambulance at the bottom of the cliff. In human medicine, immunisation is credited with averting up to 3 million deaths annually; no other health intervention better embodies the adage that an ounce of prevention is worth a pound of cure.
In the context of the global trend in antibiotic resistance, vaccines are undervalued in what they have to offer. Vaccines are a tool to help prevent the rise of antimicrobial resistance by reducing the use – and misuse – of antibiotics. Calf scours is a common and debilitating event occurring on many dairy farms every spring. These scours are largely caused by viruses, and they may or may not have a bacterial component, yet the use of an antibiotic powder for treatment is commonplace. Antibiotics do not work against viruses, but they are invariably used anyway. There are several very effective scour vaccines on the market that have been proved extremely effective, but some farmers perceive them to be too costly or prefer to take the risk. Antibiotics are used as a backup, but should they need to be? There are many more effective preventative vaccines for combatting diseases such as Salmonella, Bovine Viral Diarrhoea and respiratory disease (to name a few), all preventing viral and bacterial conditions alike.
Antibiotics are used as a backup, but should they need to be?
One of the problems with vaccines is that, if they are doing their job well, they are perceived to be unnecessary. In many ways, a good vaccine is its own worst enemy. In the sheep industry, there is vaccine protection against abortion due to Campylobacter sp. After several years of vaccination and few or no abortions, a prudent farmer may consider it unnecessary to continue with a vaccination programme. If a subsequent abortion storm were to occur, then possibly that farmer might consider treating his animals with antibiotics. This relates to the concept of herd immunity or community immunity, which means that, if enough individuals are vaccinated, then even those who are not vaccinated are less likely to get sick simply because they are less likely to encounter an individual that is sick – because those individuals have been vaccinated.
Most antibiotics used in the dairy industry are used in either the treatment or prevention of clinical mastitis. While it is hard to argue against the treatment of acute clinical mastitis on welfare grounds, the practice of using prophylactic dry cow therapy (DCT) at drying off is coming under severe scrutiny. NZVA’s policy on the use of DCT is very clear in that, by 2030, DCT will only be used in the treatment of existing intramammary infections. The use of non-antibiotic internal teat sealants has proved to be very effective at reducing peri-calving mastitis and is a good alternative for cows with no infections at drying off. While internal teat sealants have been proven to be very effective at preventing infections during the dry period and up until calving, the limitations are that, once the cow has calved, she is exposed to the common pathogens that cause mastitis. Most of the antibiotic use on dairy farms is related to the treatment of mastitis infections, so reducing this input would go a long way to reducing the risk of AMR.
What of vaccines in this area and can they be of assistance? A second mastitis vaccine, (UBAC®, for S. uberis has just become available in NZ. Sitting alongside its stablemate Startvac®. Both these vaccines work at reducing the onset of clinical cases and/or reducing the overall need for the use of antibiotics. Clearly this is one area of vaccination use that can aid and abet the course of preventing antimicrobial resistance.
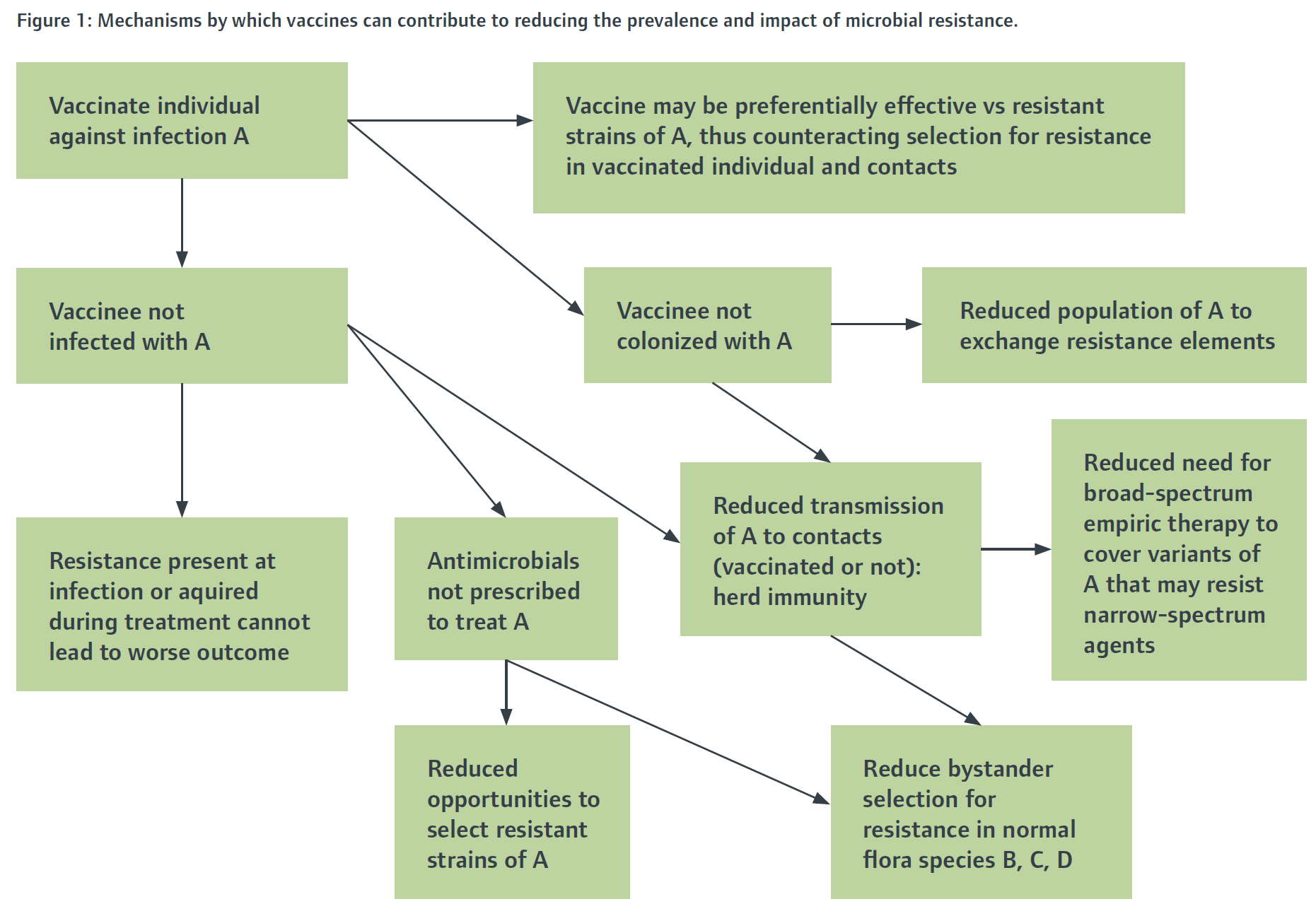
Existing vaccines already help to reduce the burden of antimicrobial resistance. Notably, in human medicine, resistance is not a significant clinical problem for either of the transmissible bacterial infections against which we have routinely vaccinated for decades (i.e. diphtheria and pertussis), most likely because they are rarely seen and thus rarely treated. Resistance was already becoming a problem in Haemophilus influenzae, Streptococcus pneumoniae (pneumococcus), and Neisseria meningitidis (meningococcus) by the time vaccines against these organisms were introduced, but the vaccines have reduced or nearly eliminated the problem. Figure 1 shows several pathways by which this may occur. Any resistant infection prevented by vaccination is a case for which, by definition, the burden of AMR disease is reduced, the need for antibiotic therapy is eliminated, and the risk of poor outcomes is avoided. Avoiding antibiotics reduces opportunities to select resistant variants of the targeted pathogen. Therefore, there is potential benefit in vaccines delivering on reducing potential AMR in farming systems.
Figure 1: Mechanisms by which vaccines can contribute to reducing the prevalence and impact of microbial resistance.
For vaccines to be taken up more readily and used to prevent disease, rather than waiting for disease and treating with antibiotics, there will need to be a shift in the mindset of many farmers and maybe some veterinarians. Cost always comes into the equation. Veterinary vaccines must be pure, safe, potent, and effective, along with being affordable, to ensure widespread use.
Generally, for the treatment of farm animals, there are plenty of good vaccines available for preventative use rather than antibiotics for therapeutic use. However, uptake is by and large very poor. Serological surveys indicate that most if not all sheep farms are infected with the protozoal infection Toxoplasmosis. However, not all farmers will vaccinate, despite serological evidence suggesting all sheep farms tested are suffering losses to Toxoplasma in some shape or form. This story is common for many vaccines and highlights the shift in thinking that will need to occur for vaccines to have an impact on AMR.
While not directly related to antimicrobial resistance, the use of vaccines as a preventative treatment may also have an impact on food safety and our export markets. Residues in food products are always of major concern, both to our trading partners and the end consumers. Most vaccines have nil withholding periods which make them inherently safe for the food chain. The use of vaccines in food-producing animals not only spares the use of antibiotics but goes a long way to removing residue risk in products, and in many ways this is helping farmers to produce more ’natural’ food. Many vaccines have registration for organic farming systems, giving a tool for these farmers to produce safe food without the use of any antibiotics. This also applies equally to conventional farming systems. The opportunities are endless.
Vaccines and antibiotics are hailed as the two greatest accomplishments of the 20th century. Vaccine usage alone is the medical intervention that has probably saved the most lives globally. As evolution begins to erode the value of antibiotics, vaccines will become a hugely valuable tool to preserve and restore this value. The greater use of vaccines in production animal systems has the potential to reduce further the reliance on antibiotics to keep animals well and keep farming sustainable and safe right through the 21st century. The tools are there in the toolbox for those brave enough to use them along with the new tools currently in production.